Gut health and mental wellness are closely linked through a bidirectional communication system known as the gut-brain axis. A healthy, diverse gut microbiome can support mood, stress resilience, and cognitive clarity, while imbalances may correspond with mood changes or fatigue. Understanding this connection helps explain everyday experiences like digestion influencing stress and mood, and vice versa.
This article explores how the gut-brain axis works, what current research suggests about mood and thinking, and practical steps you can take — through diet, probiotics and prebiotics, and lifestyle choices — to support both gut health and mental well-being.
The gut-brain axis: how two systems stay in conversation
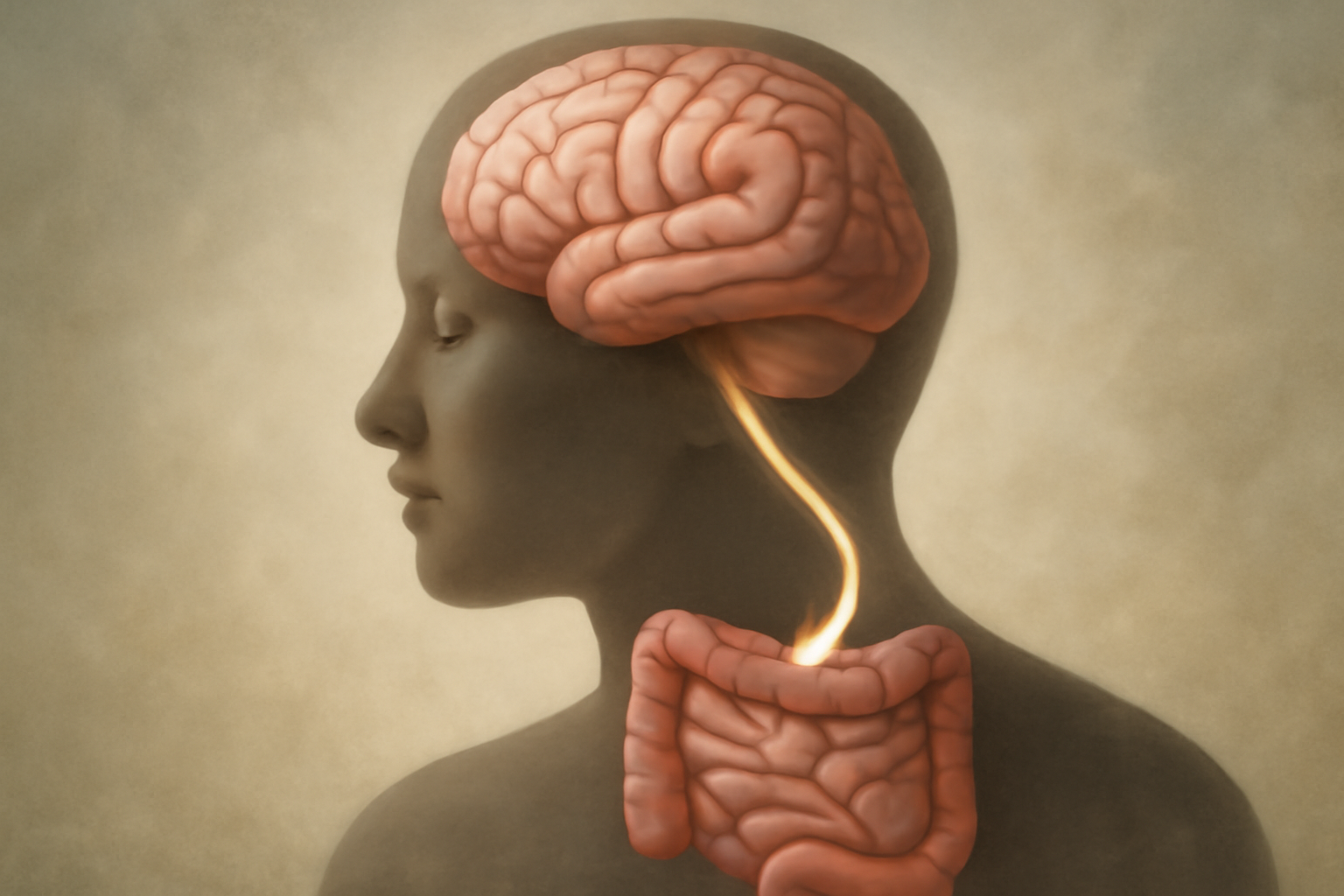
The gut-brain axis is a complex network that includes the central nervous system, the enteric nervous system (the gut’s own nervous system), the immune system, hormones, and the gut microbiome — the trillions of bacteria, fungi, and other microbes living in your digestive tract. Key communication channels include:
- The vagus nerve, a major highway for signaling between the gut and the brain
- Metabolites produced by gut bacteria, especially short-chain fatty acids like butyrate, propionate, and acetate
- Immune and inflammatory signals that travel between the gut and the brain
- Neurotransmitter precursors and hormones that influence mood and cognition
What happens in the gut can ripple to the brain, and stress or emotions can alter gut function and microbiota composition. A healthy gut ecosystem is shaped by diet, antibiotics, sleep, stress, and overall lifestyle, making gut health a practical target for mental well-being.
How gut health affects mood and cognition
Emerging evidence suggests that gut health can influence mood, anxiety, and cognitive performance in several ways. For example, gut microbes help regulate inflammation, support the production of neurotransmitter precursors, and influence the gut’s barrier integrity. When the gut microbiome is imbalanced (a state called dysbiosis), these signals may shift toward higher inflammation or altered stress responses, potentially affecting mood and thinking clarity.
In addition, gut health can impact energy, sleep, and appetite, all of which intersect with mood and cognitive function. Some people notice improvements in stress resilience or mood when they optimize fiber intake, include fermented foods, or reduce inflammatory triggers in their diet. It’s important to remember that responses are individual, and mood or cognitive changes often reflect a combination of factors beyond gut health alone.
What the research shows
Research on the gut-brain axis is rapidly evolving. Systematic reviews and meta-analyses suggest that certain probiotic strains may offer modest benefits for anxiety and depressive symptoms in specific populations, particularly those under stress or with gut-related disorders. However, effects are often small, strain-specific, and influenced by baseline health, study design, and placebo effects. More rigorous, long-term trials are needed to identify which strains help which symptoms for whom.
For readers seeking trustworthy overviews, consider sources that synthesize current findings and discuss limitations in study design and interpretation. For example, foundational work on the microbiome-gut-brain axis highlights bidirectional communication and mechanisms, while newer reviews focus on clinical implications for mood and cognition. See credible resources such as:
- Frontiers in Psychiatry — Psychobiotics and Mental Health
- Harvard Health: The Gut-Brain Connection
- NIH NICHD: Gut Microbiota and Health
- Nature Reviews Neuroscience — The Microbiome-Gut-Brain Axis
Dietary approaches to support gut health
Dietary choices profoundly shape the gut microbiome. A plant — forward, fiber-rich pattern supports microbial diversity and the production of beneficial metabolites. In parallel, fermented foods introduce live cultures that may help maintain gut balance. Consider the following evidence-based approaches as practical starting points:
Fiber and diverse plant foods
Aim for a variety of fiber sources from beans, lentils, whole grains, fruits, vegetables, nuts, and seeds. Diversity in plant-based fibers feeds a wider range of gut bacteria, promoting stability and resilience. Gradually increase fiber intake to minimize gas or bloating, and drink plenty of water to aid digestion.
Fermented foods and fermented beverages
Fermented foods like yogurt with live cultures, kefir, sauerkraut, kimchi, miso, and tempeh can introduce beneficial microbes and support gut health. If you have dietary restrictions or dairy sensitivities, there are lactose-free or plant-based fermented options available. Start with small portions and watch for tolerance.
Regular meals and mindful eating
Consistent meal timing supports the gut’s circadian rhythms and digestion. Chewing slowly and savoring meals improves digestion and may influence how nutrients reach your gut microbiome. Limiting ultra-processed foods high in added sugars and unhealthy fats can also reduce inflammatory signals from the gut.
Probiotics and prebiotics
Probiotics are live microorganisms that, in adequate amounts, may confer health benefits beyond basic nutrition. Prebiotics are nondigestible fibers that feed beneficial gut bacteria. Not all probiotics are created equal, and benefits can be strain-specific. If you’re considering supplements, talk with a clinician, especially if you have immune concerns or complex medical conditions.
What to know about probiotics
- Look for products with well-studied strains and clear labeling of colony — forming units (CFUs) and viability through expiration.
- Commonly studied strains include Lactobacillus and Bifidobacterium species; however, effects on mood and cognition vary by strain and individual.
- Probiotics can interact with medications or medical conditions, so professional guidance is wise before starting a new supplement regimen.
What to know about prebiotics
- Key prebiotic fibers include inulin, galactooligosaccharides (GOS), resistant starch, and certain pectins found in fruits.
- Prebiotics help diversify gut bacteria and support their metabolite production, which can influence gut and brain signaling.
- Introduce prebiotics gradually to reduce gas and discomfort, especially if your current diet is low in fiber.
Useful external reads for deeper dives into probiotics and prebiotics include peer-reviewed syntheses and clinical summaries. See resources such as:
Lifestyle factors that support gut health
Beyond diet, lifestyle plays a crucial role in shaping the gut microbiome and, by extension, mental wellness. Consider these evidence-informed factors:
- Sleep quality: Regular, sufficient sleep supports gut motility, microbial balance, and stress regulation.
- Physical activity: Regular exercise is associated with greater microbial diversity and a more resilient gut ecosystem.
- Stress management: Mindfulness, breathing exercises, yoga, and other stress-reduction practices can dampen gut-related inflammation and improve digestion.
- Antibiotic stewardship: Use antibiotics only when prescribed and necessary; discuss alternatives or finish the course as directed, since antibiotics can disrupt gut bacteria.
- Substance use: Smoking cessation and moderating alcohol intake support a healthier gut environment.
Practical strategies for improving gut health
Turning science into everyday habits can be straightforward. Use this starter plan to begin optimizing gut health while supporting mental well-being:
- Week 1: Increase fiber gradually. Add one new plant-based fiber source every few days (e.g., beans, oats, berries). Aim for a daily total of 25–38 grams of fiber, adjusting to your tolerance.
- Week 2: Introduce fermented foods. Include one serving of yogurt, kefir, sauerkraut, kimchi, miso, or tempeh daily. If dairy-free, choose plant-based options with live cultures.
- Week 3: Nurture prebiotics. Add prebiotic-rich foods like onions, garlic, bananas, asparagus, and Jerusalem artichokes, along with legumes and whole grains. Increase gradually to avoid gastrointestinal discomfort.
- Hydration and mindful eating. Drink water consistently throughout the day and chew meals thoroughly to support digestion and nutrient absorption.
- Sleep and stress routine. Prioritize 7–9 hours of sleep and practice a 10-minute daily stress-management technique such as breathing exercises or a short mindfulness session.
- Activity and routine. Incorporate at least 150 minutes of moderate activity per week, plus a couple of short resistance sessions to support overall health and microbiome diversity.
- Monitor and adjust. Track mood, energy, sleep, digestion, and stress. If you notice persistent GI symptoms, significant mood changes, or if you’re considering probiotics, consult a healthcare professional for personalized guidance.
Special considerations: if you’re pregnant, immunocompromised, have chronic GI conditions, or are taking medications that affect gut function, speak with a clinician before making major dietary changes or starting supplements. While gut health is a meaningful piece of mental wellness, it is one part of a broader health picture that includes sleep, exercise, social connection, and medical care when needed.
⚠️ This content is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed physician, psychiatrist, psychologist, or other qualified healthcare professional before making decisions about medications, mental health treatment, or alternative and holistic treatment.

